There’s a reason why people say, “calm down or you’re going to have a heart attack.”
Chronic stress, brought on by your job, money, or relationship trouble, is suspected to increase the risk of a heart attack. Researchers are now studying harried medical residents and harassed rodents, and have offered an explanation for how, at a physiological level, long-term stress can endanger the cardiovascular system as it revolves around immune cells that circulate in the blood.

Studying the effect of stressful intensive care unit (ICU) shifts on medical residents, biologist Matthias Nahrendorf of Harvard Medical School in Boston recently found that blood samples taken when the doctors were most stressed out had the highest levels of neutrophils and monocytes. To investigate whether these white blood cells are the missing link between stress and atherosclerosis, he and his colleagues turned to doing experiments on mice.
Nahrendorf’s team exposed mice for up to 6 weeks to stressful situations, including tilting their cages, rapidly alternating light with darkness, or regularly switching the mice between isolation and crowded quarters. Compared with control mice, the stressed mice had increased levels of neutrophils and monocytes in their blood. The researchers then homed in on an explanation for the higher levels of immune cells. They already knew that chronic stress increases the hormone noradrenaline, which binds to a cell surface receptor protein called ?3 on stem cells in the bone marrow. In turn, the chemical environment of the bone marrow changes and there’s an increase in the activity of the white blood cells produced by the stem cells. When the scientists blocked the ?3 receptor, though, stressed mice not only had fewer of these dangerous plaques, but also had reduced levels of the active immune cells in their plaques, pinpointing ?3 as a key link between stress and atherosclerosis.
“It makes sense that stress wakes up these immune cells because an enlarged production of leukocytes prepares you for danger, such as in a fight, where you might be injured,” Nahrendorf says. “But chronic stress is a different story – there’s no wound to heal and no infection.”
The new observations suggest a way that clinicians could screen patients for their risk of atherosclerosis, heart attack and stroke, Tall says. “Rather than asking four questions about stress levels, we could use their white blood cell counts to monitor psychosocial stress,” he says. The new finding is “surprising,” says physician and atherosclerosis researcher Alan Tall of Columbia University, who was not involved in the new study. “The idea has been out there that chronic psychosocial stress is associated with increased cardiovascular disease in humans, but what’s been lacking is a mechanism,” he notes.
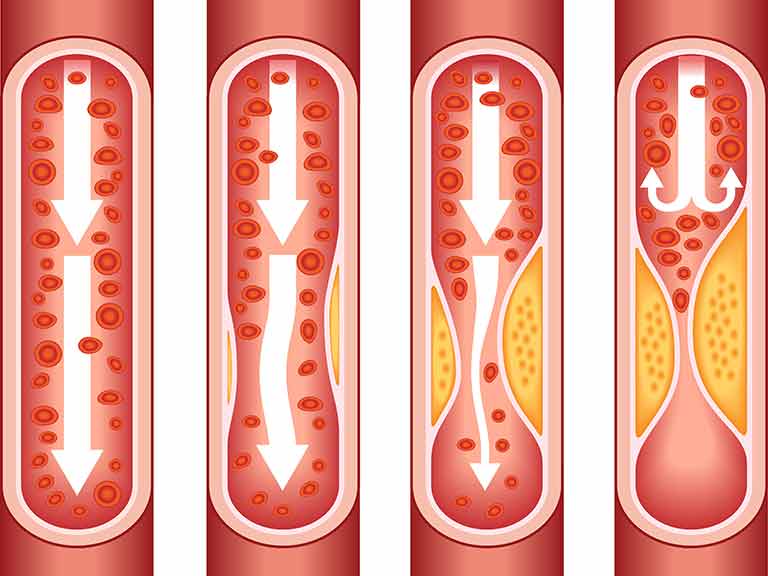
Epidemiological studies have shown that people who face many stressors, from those who survive natural disasters to those who work long hours, are more likely to develop atherosclerosis, the accumulation of fatty plaques inside blood vessels. In addition to fats and cholesterol, the plaques contain monocytes and neutrophils, immune cells that cause inflammation in the walls of blood vessels. And when the plaques break loose from the walls where they’re lodged, they can cause more extreme blockages elsewhere leading to a stroke or heart attack.
Reference:
Heidt, T. et al., Chronic variable stress activates hematopoietic stem cells, Journal of Nature Medicine, 2014. 20: p. 754 – 758
